The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is one of the most significant changes in healthcare reimbursement in the past few decades. It gave rise to the Quality Payment Program, which has two tracks:
- The Merit-based Incentive Payment System (MIPS)
- Advanced Alternative Payment Models
MIPS Overview
The majority of MIPS eligible providers will be under MIPS in 2019 and 2020, and likely 2021. CMS is gradually increasing the MIPS thresholds needed to avoid future negative payment adjustments. In 2019 the performance threshold is set at 30 points. It is projected to go to 45 points in 2020 and 60 points in 2021. In 2022 the performance threshold will be based on the mean or median score for all practices. Based on current performance this would likely be above 80 points.
Practices that score above the performance threshold earn a positive payment adjustment applied to Medicare Part B claims in the corresponding payment year, which is always two years after the performance year. Positive payment adjustment may reach as high as +7% based on 2019 performance, and as high as +9% starting in 2020 and for future years. Practices that score below the payment threshold may receive negative payment adjustments of up to 7%. Starting in 2020 this number increases to -9%.
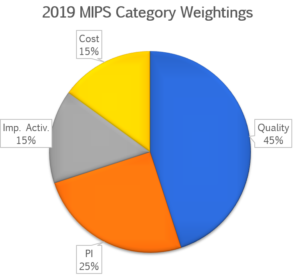
The MIPS score is based on performance in 4 performance categories:
- Quality: for more information see: MIPS Quality Performance Category
- Promoting Interoperability: for more information see:
- Cost: for more information see: 2019 Cost Performance Category Fact Sheet
- Improvement Activities: for more information see: 2019 Improvement Activities Fact Sheet_Final
For physicians and groups that include physicians the 4 categories have the following weightings:
Weightings may change base on clinician type, practice setting, exclusions and other factors.
Advanced Alternative Payment Model Overview
Clinicians that participate in an Advanced APM and that reach minimum thresholds for APM attributed patients or revenue achieve the status of “Qualifying Participants.” This individuals are excluded from the MIPS and receive a 5% lump sum bonus payment (based on Medicare Part B payments) during the corresponding payment year.
There are relatively few opportunities for clinicians to participate in Advanced APMs, although new models are being developed and tested. In 2019 CMS approved the use of Medicare/Medicaid Advanced APMs, and private payer combination Advanced APMs.
The following is a list of Advanced Alternative Payment Models approved by CMS for 2019
| Bundled Payments for Care Improvement (BPCI) Advanced | The Bundled Payments for Care Improvement (BPCI) initiative is a model of care, which links payments for the multiple services beneficiaries receive during a clinical episode of care. |
| Comprehensive ESRD Care (CEC) – Two-Sided Risk | The Comprehensive ESRD Care (CEC) Model is designed to identify, test, and evaluate new ways to improve care for Medicare beneficiaries with End-Stage Renal Disease (ESRD). |
| Comprehensive Primary Care Plus (CPC+) | Comprehensive Primary Care Plus (CPC+) is a national advanced primary care medical home model that aims to strengthen primary care through regionally-based multi-payer payment reform and care delivery transformation. |
| Medicare Accountable Care Organization (ACO) Track 1+ Model | The Medicare ACO Track 1+ is a time-limited model for Track 1 Medicare Shared Savings Program (Shared Savings Program) ACOs. The Shared Savings Program is a voluntary program that encourages groups of doctors, hospitals, and other health care providers to come together as an ACO to provide coordinated, high-quality care to their Medicare patients. Track 1+ Model ACOs assume limited downside risk (less than Track 2 or Track 3). |
| Next Generation ACO Model | Building upon experience from the Pioneer ACO Model and the Shared Savings Program, the Next Generation ACO Model offers a new opportunity in accountable care—one that sets predictable financial targets, enables providers and beneficiaries greater opportunities to coordinate care, and aims to attain the highest quality standards of care. |
| Medicare Shared Savings Program – Tracks 2 and 3 | The Shared Savings Program is a voluntary program that encourages groups of doctors, hospitals, and other health care providers to come together as an ACO to provide coordinated, high-quality care to their Medicare patients. Track 2 and 3 ACOs may share in savings or repay Medicare losses depending on performance. Track 2 ACOs may share in a greater portion of savings than Track 1 ACOs. Track 3 ACOs take on the greatest amount of risk but may share in the greatest portion of savings if successful. |
| Oncology Care Model (OCM) – Two-Sided Risk | Under the Oncology Care Model (OCM), physician practices have entered into payment arrangements that include financial and performance accountability for episodes of care surrounding chemotherapy administration to cancer patients. |
| Comprehensive Care for Joint Replacement (CJR) Payment Model (Track 1-CEHRT) | The Comprehensive Care for Joint Replacement (CJR) model aims to support better and more efficient care for beneficiaries undergoing the most common inpatient surgeries for Medicare beneficiaries: hip and knee replacements (also called lower extremity joint replacements or LEJR). |
| Vermont Medicare ACO Initiative (as part of the Vermont All-Payer ACO Model) | The Vermont All-Payer Accountable Care Organization (ACO) Model is the Centers for Medicare & Medicaid Services’ (CMS) new test of an alternative payment model in which the most significant payers throughout the entire state – Medicare, Medicaid, and commercial health care payers – incentivize health care value and quality, with a focus on health outcomes, under the same payment structure for the majority of providers throughout the state’s care delivery system and transform health care for the entire state and its population. |
| Comprehensive ESRD Care (CEC) Model | The Comprehensive ESRD Care (CEC) Model is designed to identify, test, and evaluate new ways to improve care for Medicare beneficiaries with End-Stage Renal Disease (ESRD). Through the CEC Model, CMS partners with health care providers and suppliers to test the effectiveness of a new payment and service delivery model in providing beneficiaries with person-centered, high-quality care. |
| Maryland All-Payer Model (Care Redesign Program) | The Care Redesign Program (CRP) is a voluntary program within the Maryland All-Payer Model that advances efforts to redesign and better coordinate care in Maryland. The CRP provides hospitals participating in the Maryland All-Payer Model the opportunity to partner with and provide incentives and resources to certain providers. In exchange, suppliers offer activities and processes that aim to improve quality of care and reduce the growth in total cost of care for Maryland Medicare beneficiaries. |
| Maryland Total Cost of Care Model (Maryland Primary Care Program) | The Maryland Total Cost of Care Model builds on the success of the Maryland All-Payer Model by creating greater incentives for health care providers to coordinate with each other and provide patient-centered care, and by committing the State to a sustainable growth rate in per capita total cost of care spending for Medicare beneficiaries. |
| Maryland Total Cost of Care Model (Care Redesign Program) | The Care Redesign Program (CRP) allows hospitals to make incentive payments to non-hospital health care providers who partner and collaborate with the hospital and perform care redesign activities aimed at improving quality of care. A participating hospital may only make incentive payments if it has attained certain savings under its fixed global budget and the total amount of incentive payment made cannot exceed such savings. |
For additional information see the CMS Quality Payment Program information site on Advanced APMs